Prescribing information (external link)
![Hero banner. LUTATHERA® (lutetium [177Lu] oxodotreotide) logo. Hero banner. LUTATHERA® (lutetium [177Lu] oxodotreotide) logo.](/uk-en/sites/pro_novartis_com_uk/files/styles/twoup_layout_desktop_1080/public/2025-08/lutathera-home-hero-banner-hcp-2700_0.png.webp?itok=KiWg7nHk)
![Hero banner. LUTATHERA® (lutetium [177Lu] oxodotreotide) logo. Hero banner. LUTATHERA® (lutetium [177Lu] oxodotreotide) logo.](/uk-en/sites/pro_novartis_com_uk/files/styles/twoup_layout_desktop_1080/public/2025-08/lutathera-home-hero-banner-hcp-1000_0.png.webp?itok=cL3k8yXL)
Identifying progression
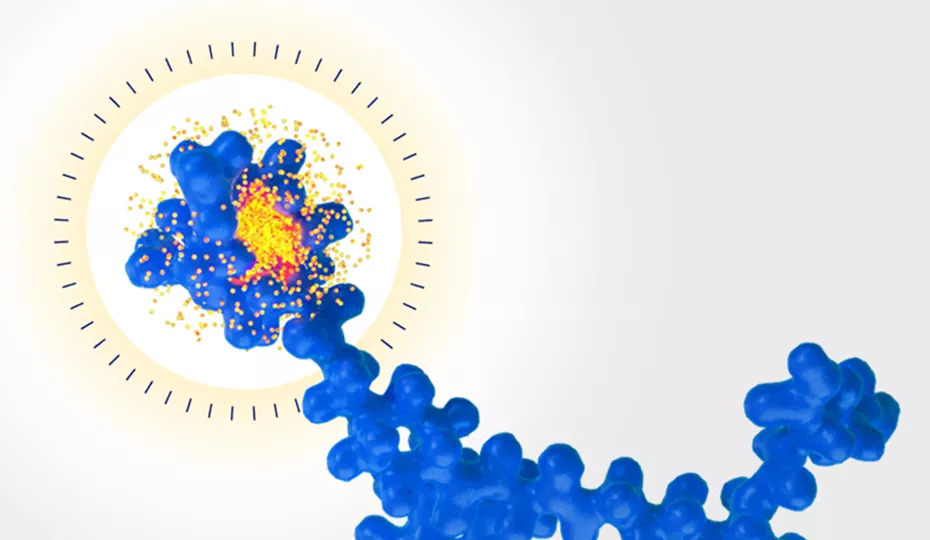
LUTATHERA® (lutetium [177Lu] oxodotreotide) is indicated for the treatment of unresectable or metastatic, progressive, well-differentiated (G1 and G2), somatostatin receptor (SSTR)-positive gastroenteropancreatic neuroendocrine tumours (GEP-NETs) in adults.1
LUTATHERA® Summary of Product Characteristics (SmPC) can be found here
Disease progression in GEP-NETs affects overall survival and quality-of-life2,3
Although sometimes considered slow-growing, most GEP-NETs ultimately progress despite treatment and may cause death.4–8
Identification of progression is essential to improve patient outcomes by providing an opportunity to change treatment. In clinical practice, multiple factors are considered when deciding when to change therapy, including:9,10
Tumour burden

Drug-related toxicity

Cancer-related symptoms
Recurrent or worsening symptoms may indicate disease progression11
Clinical (symptomatic) progression may occur alone or in conjunction with radiological progression.12
Patients with GEP-NETs may experience symptoms due to increased tumour burden or secretion of bioactive substances from functional tumours11–13
Assessment of signs and symptoms may suggest disease progression and therefore prompt imaging scans and other laboratory tests11
Potential symptoms due to:
Functional carcinoid tumours12
Patients with functional NETs may suffer increased episodes of:
Increased tumour burden12
Patients may experience:
This is not an exhaustive list of symptoms. Different types of hormones may cause other rare symptoms. For a full list of possible symptoms, please visit www.cancer.net/cancer-types/neuroendocrine-tumors/symptoms-and-signs.
Assessment of tumour burden frequently requires multiple imaging modalities as well as clinical assessment:14
Computer tomography (CT) scan
Magnetic resonance imaging (MRI) scan
SSTR imaging
Contrast-enhanced ultrasound
Endoscopic ultrasound
Fluorodeoxyglucose positron emission tomography
Clinical trials vs clinical practice
RECIST* criteria provide standardised assessments for clinical trials, but may not impact clinical decision-making.15 With the spontaneous, slow evolution of GEP-NETs, RECIST criteria may classify stable disease even when some progression has occurred.11
Biomarkers
Chromogranin A (CgA) is a marker for GEP-NETs, irrespective of functional status16
5-hydroxyindoleacetic acid (5-HIAA) is a marker for functional NETs13,17
Guidelines offer monitoring recommendations for patients with well-differentiated GEP-NETs
These links will take you to the ENETS/ESMO websites, which are non-Novartis websites.
European Neuroendocrine Tumor Society (ENETS)
ENETS 2023 guidance paper for gastroduodenal neuroendocrine tumours (NETs)18
ENETS 2024 guidance paper for the management of well-differentiated small intestine neuroendocrine tumours19
ENETS 2023 guidance paper for functioning pancreatic neuroendocrine tumour syndromes20
ENETS 2023 guidance paper for non-functioning pancreatic neuroendocrine tumours21
ENETS 2023 guidance paper for colorectal neuroendocrine tumours22
ENETS 2023 guidance paper for appendiceal neuroendocrine tumours23
ENETS consensus guidelines for high-grade gastroenteropancreatic neuroendocrine tumors and neuroendocrine carcinomas24
European Society for Medical Oncology (ESMO)
Gastroenteropancreatic neuroendocrine neoplasms: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up25
If you are referring your eligible patient for LUTATHERA®, consider the following:
Do you have the patient’s full medical history?
Presentation, diagnosis, histopathology, tumour characteristics, performance status, current and previous treatments/surgery, comorbidities, date of last somatostatin analogue (SSA).
SSAs competitively bind to SSTRs and may interfere with the efficacy of LUTATHERA®. Therefore, administration of long-acting SSAs should be avoided within 30 days prior to the administration of this medicinal product. If necessary, patients may be treated with short-acting SSAs up to 24 hours preceding LUTATHERA® administration.1
What are the patient’s haematology results?
Haemoglobin, absolute neutrophil count, platelets.
What are the patient’s tumour markers?
CgA/CgB, 5-HIAA, gut hormones.
What is the evidence of progression?
Symptoms, biochemistry, imaging on CT/MRI, imaging on SSTR.
Are routine biochemistry assessments complete?
Urea and electrolytes, glucose levels, liver function tests, thyroid, bone, albumin.
What is their current cardiac status?
Echocardiogram and NT-proBNP within 3–6 months.
Do you have the patient’s background information?
Family members, specific personal or medical requirements, safeguarding concerns, emergency contact, ability to consent, childbearing potential/pregnancy.
*An increase of ≥20% in the sum of diameters of target lesions, compared with the smallest sum on study (including the baseline if that is the smallest on study); the sum must also demonstrate an increase of ≥5 mm, and/or the appearance of one or more new lesions.11
5-HIAA, 5-hydroxyindoleacetic acid; Cg, chromogranin; CT, computed tomography; ENETS, European Neuroendocrine Tumor Society; ESMO, European Society for Medical Oncolog; GEP-NET, gastroenteropancreatic neuroendocrine tumour; MRI, magnetic resonance imaging; NT-proBNP, pro-B-type natriuretic peptide; RLT, radioligand therapy; SmPC, summary of product characteristics; SSA, somatostatin analogue; SSTR, somatostatin receptor.
References
LUTATHERA® Summary of Product Characteristics.
Ter-Minassian M, et al. Oncologist 2017;22(2):165–172.
Strosberg J, et al. J Clin Oncol 2018;36(25):2578–2584.
Arnold R, et al. Clin Gastroenterol Hepatol 2005;3(8):761–771.
Rinke A, et al. J Clin Oncol 2009;27(28):4656–4663.
Rinke A, et al. Neuroendocrinology 2017;104(1):26–32.
aplin ME, et al. Endocr Relat Cancer 2016;23(3):191–199.
Capdevila J, et al. Oncologist 2019;24(12):e1315–e1320.
Oxnard GR, et al. J Natl Cancer Inst 2012;104(20):1534–1541.
Merino-Casabiel X, et al. Clin Transl Oncol 2018;20(12):1522–1528.
de Mestier L, et al. Endocr Relat Cancer 2014;21(3):R105–R120.
Toumpanakis C, et al. Aliment Pharmacol Ther 2009;30(7):733–740.
Riechelmann RP, et al. Ther Adv Med Oncol 2017;9(2):127–137.
Maxwell JE & Howe JR. Int J Endocr Oncol 2015;2(2):159–168.
Eisenhauer EA, et al. Eur J Cancer 2009;45(2):228–247.
Oberg KE. Clin Oncol (R Coll Radiol) 2012;24(4):282–293.
Kocha W, et al. Curr Oncol 2010;17(3):49–64.
Panzuto F, et al. J Neuroendocrinol 2023;35(8):e13306.
Lamarca A, et al. J Neuroendocrinol 2024;36(9):e13423.
Hofland J, et al. J Neuroendocrinol 2023;35(8):e13318.
Kos-Kudła B, et al. J Neuroendocrinol 2023;35(12):e13343.
Rinke A, et al. J Neuroendocrinol 2023;35(6):e13309.
Kaltsas G, et al. J Neuroendocrinol 2023;35:e13332.
Garcia-Carbonero R, et al. Neuroendocrinology 2016;103:186–194.
Pavel M, et al. Ann Oncol 2020;31(7):844–860.
UK | December 2025 | FA-11464153
Adverse events should be reported. Reporting forms and information can be found at www.mhra.gov.uk/yellowcard. Adverse events should also be reported to Novartis online through the pharmacovigilance intake (PVI) tool at www.novartis.com/report, or alternatively email [email protected] or call 01276 698370.