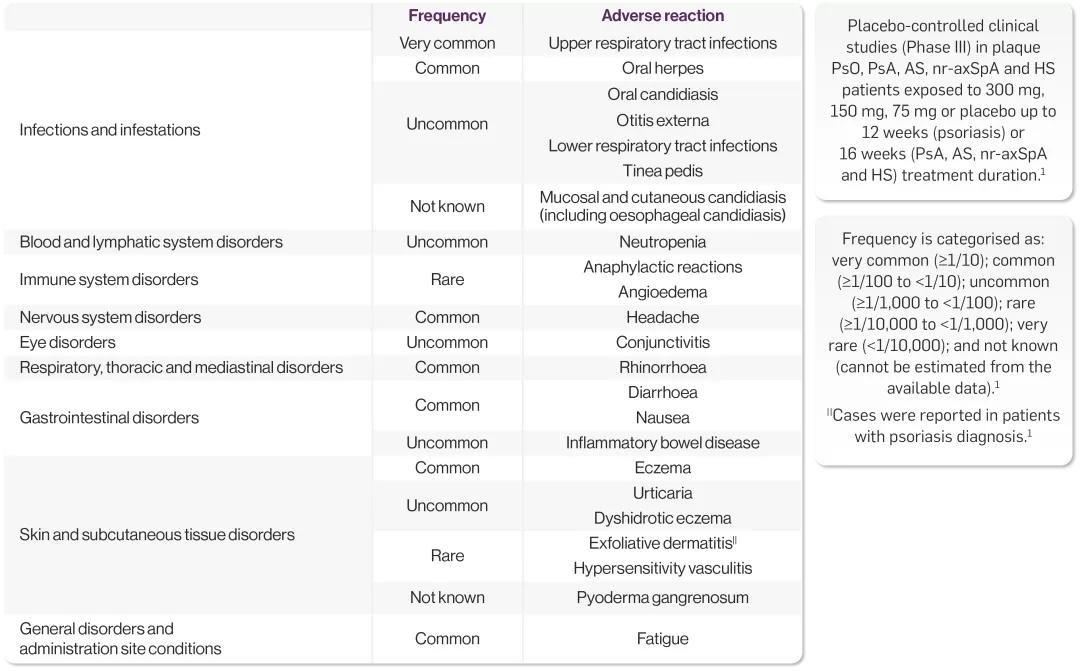
AE, adverse event; AS, ankylosing spondylitis; EAIR, exposure-adjusted incidence rate; ERA, enthesitis-related arthritis; HBV, hepatitis B virus; HLT, high-level term; HS, hidradenitis suppurativa; IBD, inflammatory bowel disease; IGA, investigator global assessment; JPsA, juvenile psoriatic arthritis; MACE, major adverse cardiovascular event; MTX, methotrexate; nr-axSpA, non-radiographic axial spondyloarthritis; NRS30, numeric rating scale 30; NMQ, Novartis MedDRA query; PASI, psoriasis area and severity index; PsA, psoriatic arthritis; PsO, plaque psoriasis; Q2W, every 2 weeks; Q4W, every 4 weeks; RWE, real-world evidence; SAE, serious adverse event; SmPC, summary of product characteristics; SMQ, standardised MedDRA queries; SOC, standard of care; URTI, upper respiratory tract infection.