Contact
Novartis Pharma NV/SA:
+ 32 (0)2 246 16 11
In case of an adverse event:
[email protected]
Phone number 24/h:
Bel: 0800 94 368
Lux: + 32 475 319 792
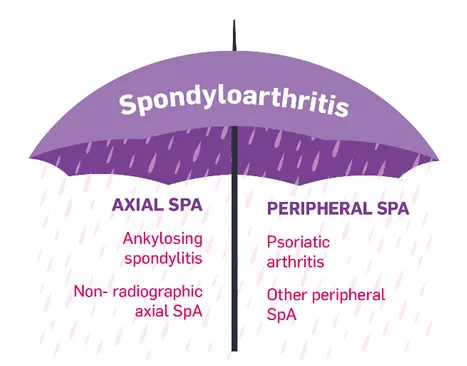
Psoriatic arthritis (PsA), is a chronic, progressive inflammatory disease. PsA causes painful, swollen, and stiff joints1. It is one of a group of conditions called spondyloarthritis, which is a term used to describe various types of arthritis caused by inflammation.
Without proper treatment, PsA can get worse, which is known as a PsA flare. If it is left untreated, PsA can cause permanent joint damage2,3.
PsA is equally common in men and women4. It can occur at any age, but most people develop it when they are around 40-50 years old5. Sometimes it can also start in childhood6.
PsA is more likely to occur in people who already have psoriasis, which is an inflammatory skin condition that causes thick, raised, scaly patches4. Around one in five people with psoriasis also have PsA7. PsA is particularly likely to develop in people who have psoriasis in their nails, scalp, or around their anus8, and in people who have psoriasis in multiple areas of their body5.
Most people with both PsA and psoriasis have psoriasis for a long time before developing joint problems. Around 15 in every 100 people with both conditions develop PsA first, and another 15 in every 100 develop both psoriasis and PsA at the same time4.
PsA can affect different parts of the body, including1:
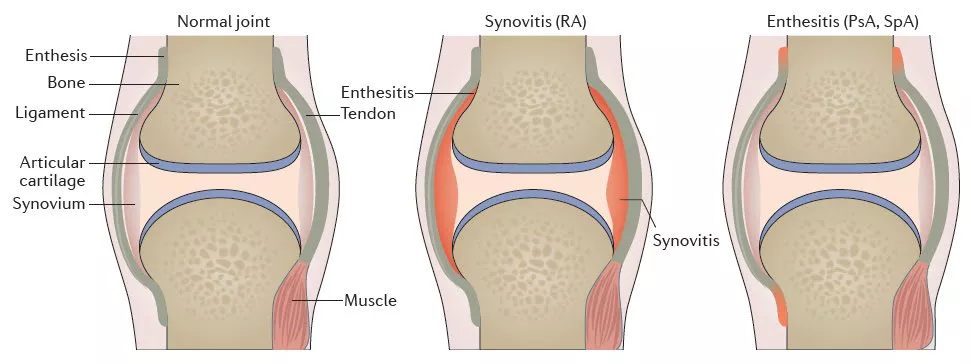
PsA is not caused by overuse of joints or aging. It is an autoimmune disease, meaning the immune system, which normally protects against infections, attacks the body’s own tissues. Inflammatory proteins called cytokines are released, which cause inflammation and damage, in this case to the joints1,4. PsA seems to develop due to a combination of genetic, immunological, and environmental factors1,4.
Genetic factors
Around four in 10 people with psoriasis or PsA have a family history of one or either disease4. The risk of developing PsA if a family member also has it is around the same as the risk of developing PsA for someone who already has psoriasis4. Particular genes are linked to an increased risk of developing PsA, and also to the severity of the disease1,4.
Immunological factors
People with PsA have an overactive immune system. This includes increased numbers of specific proteins (cytokines) that drive inflammation, triggering an anti-inflammatory cascade. This cascade leads to joint inflammation and damage1,4. In people who have a genetic risk, environmental factors can trigger this immune inflammatory response1,4.
Environmental factors
Environmental factors can trigger PsA in patients with a genetic risk. These factors include imbalance in the gut microbiome, obesity, mechanical stress or injury to joints, smoking, and certain infections (including streptococcal and HIV infection)1,4.
Healthcare professionals: Register now to access up-to-date information about PsA treatment.