Contact
Novartis Pharma NV/SA:
+ 32 (0)2 246 16 11
In case of an adverse event:
[email protected]
Phone number 24/h:
Bel: 0800 94 368
Lux: + 32 475 319 792
PsA is diagnosed by a rheumatologist assessing symptoms, performing a physical examination of the joints, and reviewing medical and family history1. Blood tests and analysis of joint fluid can show inflammation and rule out other diagnoses1. The rheumatologist may also do X-rays and in some cases, MRI scans to assess joint damage and soft tissue inflammation1.
If PsA is suspected in an individual, their healthcare professional should promptly refer them to a rheumatologist. Healthcare professionals may also need to work together with experts in PsA, particularly when patients have common conditions that occur alongside PsA, such as psoriasis. Dermatologists should proactively monitor patients with psoriasis for signs of joint or arthritic involvement, to help with early detection of PsA2.
Early referral and diagnosis are essential in PsA. Delayed diagnosis of PsA results in worse physical function3,4. Even a six-month delay can result in worse outcomes for patients, with more joint erosion and damage5, and an increased frequency of comorbidities (other medical conditions that occur at the same time as the primary diagnosis)5. These can include obesity, cardiovascular disease, and depression5.
PsA may share features with other types of spondyloarthritis, and with osteoarthritis and rheumatoid arthritis. Features that suggest PsA rather than other conditions are joint erosion seen on X-ray, synovitis (inflammation of the joint linings) seen on power doppler ultrasound, and a personal or family history of psoriasis6. Patients with PsA are less likely to have autoantibodies (antibodies made against the body’s own proteins) called rheumatoid factor and anticitrullinated protein antibodies6. These antibodies are typically associated with rheumatoid arthritis6.
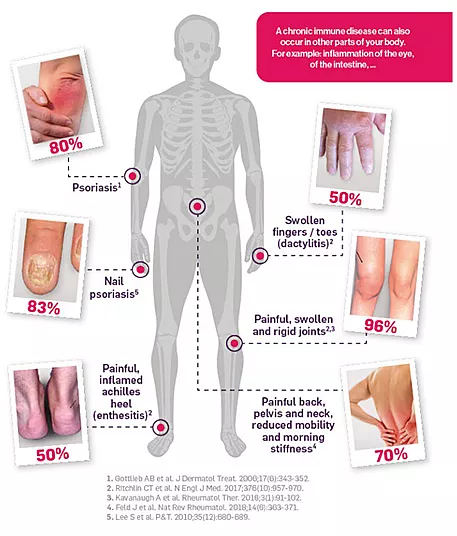
People with PsA have a higher risk of developing inflammatory conditions outside the joints, including inflammatory bowel disease, uveitis (eye inflammation), depression, cardiovascular diseases, and metabolic syndrome (a grouping of high blood pressure, high blood sugar, and obesity)1.
Healthcare professionals: Register now to access up-to-date information about PsA treatment.