Hortobagyi GN, et al. N Engl J Med. 2022;386(10):942–950
Neven P, et al. Breast Cancer Res. 2023;25:103.
Lu Y-S, et al. Clin Cancer Res. 2022;28:851–859.
Yardley DA, et al. Ann Oncol. 2022;33(S7):S629.
Im S-A, et al. N Engl J Med. 2019;381:307–316.
Hortobagyi GN, et al. N Engl J Med. 2016;375(18):1738–1748.
Slamon DJ, et al. J Clin Oncol. 2018;36(24):2465–2472.
KISQALI (ribociclib). Prescribing Information.
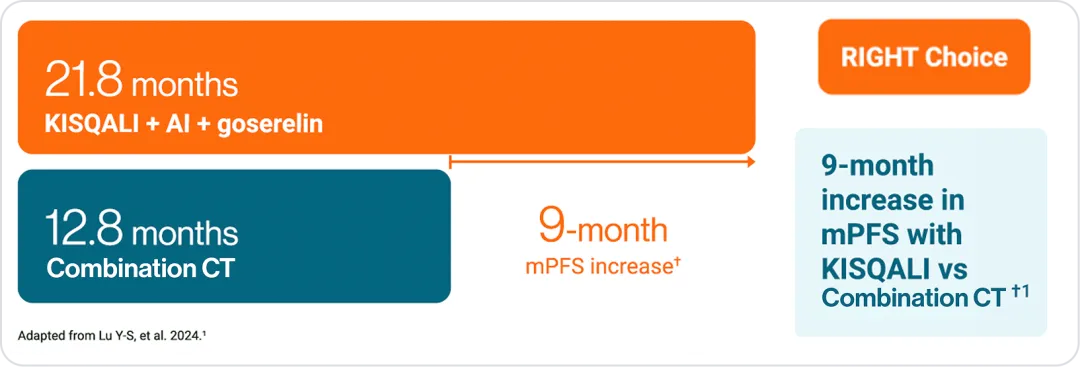
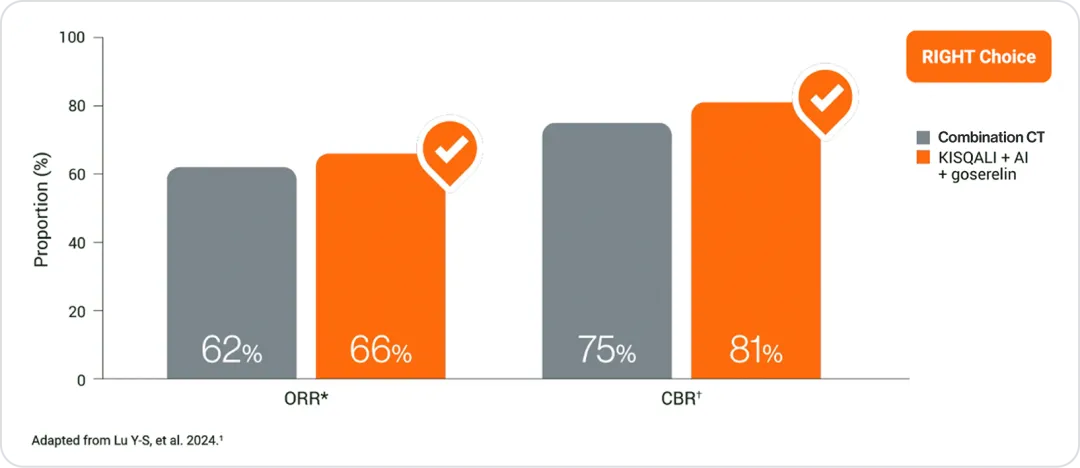
Lu Y-S, et al. J Clin Oncol. 2024;42(23):2812–2821.
Lu Y-S, et al. J Clin Oncol. 2024;42(23):2812–2821.
Hortobagyi GN, et al. N Engl J Med. 2022;386(10):942–950.
Slamon DJ, et al. Ann Oncol. 2021;32(8):1015–1024.
Lu Y-S, et al. Clin Cancer Res. 2022;28:851–859.
Yardley D, et al. ESMO 2022. Poster 205P.
Hortobagyi GN, et al. N Engl J Med. 2016;375(18):1738–1748.
Slamon DJ, et al. J Clin Oncol. 2018;36(24):2465–2472.
KISQALI (ribociclib). Prescribing Information.
Verma S, et al. Br Cancer Res Treat. 2018;170:535–545.
Beck JT, et al. Cancer Res. 2019;79 (4_Supplement):P6-18-14.
Fasching PA, et al. The Breast. 2020;54:148–154.
Harbeck M, et al. Ther Adv Med Oncol. 2020;12:1–8 (Supplement).
Hortobagyi GN, et al. N Engl J Med. 2016;375(18):1738–1748.
Slamon DJ, et al. J Clin Oncol. 2018;36(24):2465–2472.
Lu Y-S, et al. Clin Cancer Res. 2022;28:851–859.
KISQALI (ribociclib). Prescribing Information.
Eralp Y, et al. Poster presentation 456P. Presented at European Society for Medical Oncology 2023, 20–24 October, Madrid, Spain.
Lu Y-S, et al. J Clin Oncol. 2024;42(23):2812–2821.
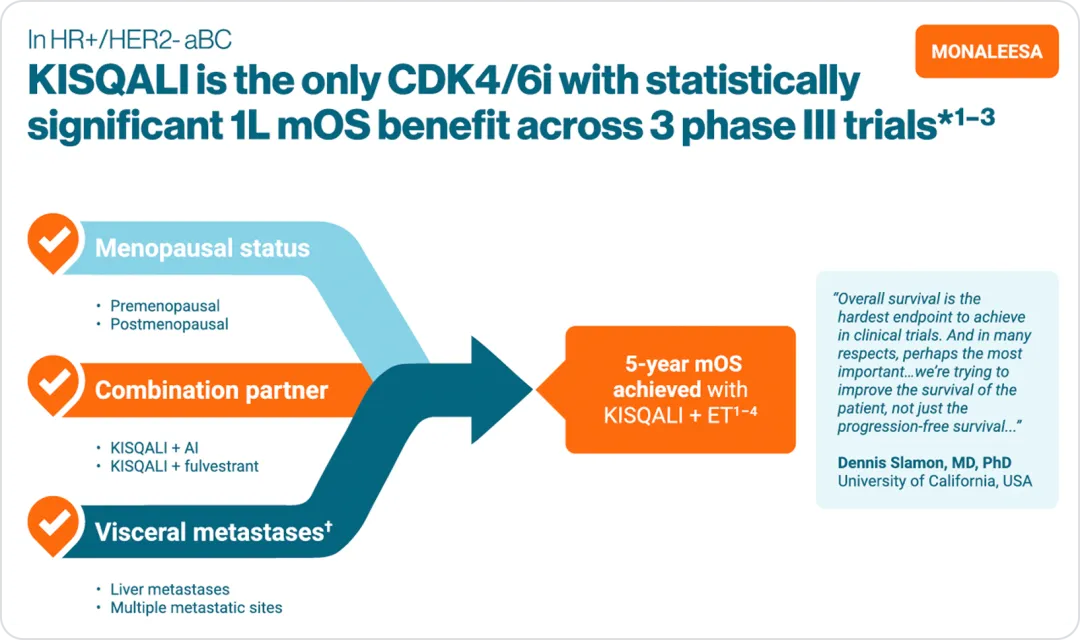
OS benefit
MONALEESA-2: N=668, double-blind, placebo-controlled, 1:1 randomised, multicentre, phase III trial in postmenopausal women with HR+/HER2− aBC. As 1L in advanced disease. No prior ET for aBC and no previous systemic chemotherapy for advanced disease. KISQALI® 600 mg or placebo orally once daily (3 weeks on/1 week off)
+ AI (letrozole 2.5 mg continuous). The primary endpoint was locally assessed PFS, and the key secondary endpoint was OS. Other secondary endpoints included the ORR (complete or partial response), the CBR (overall response plus stable disease lasting 24 weeks or more), safety, and QoL assessments.1,6
MONALEESA-3: N=726, double-blind, placebo-controlled, 2:1 randomised, phase III trial. As 1L and 2L in advanced disease plus those with early relapse in postmenopausal women with HR+/HER2– aBC. KISQALI® 600 mg or placebo orally once daily (3 weeks on/1 week off) + 500 mg intramuscular fulvestrant. The primary endpoint was locally assessed PFS. Secondary endpoints included OS, ORR, CBR, and safety and tolerability. 1L defined as: Newly diagnosed (de novo) aBC patients or patients with relapse >12 months from completion of neoadjuvant ET with no treatment for aBC or metastatic disease.2,7
MONALEESA-7: N=672, double-blind, placebo-controlled, 1:1 randomised, phase III trial in pre- or perimenopausal women with HR+/HER2− aBC. As 1L in advanced disease and in patients who received 1 or fewer lines of chemotherapy for aBC. KISQALI® 600 mg or placebo orally once daily (3 weeks on/1 week off) + AI (letrozole 2.5 mg or anastrozole 1 mg) or tamoxifen* 20 mg orally once daily continuously + LHRH agonist (goserelin 3.6 mg subcutaneously on day 1 of everycycle). The primary endpoint was investigator-assessed PFS. The key secondary endpoint was OS, defined as the time from randomisation to death from any cause.3
KISQALI® should not be co-administered with tamoxifen.8
1L, first-line; 2L, second-line; aBC, advanced breast cancer; AI, aromatase inhibitor; CBR, clinical benefit rate; CDK4/6i, cyclin-dependent kinase 4 and 6 inhibitor; CI, confidence interval; ET, endocrine therapy; HER2-, human epidermal growth factor receptor 2 negative; HR, hazard ratio; HR+, hormone receptor positive; LHRH, luteinising hormone-releasing hormone; mOS, median overall survival; ORR, overall response rate; OS, overall survival; PFS, progression-free survival; QoL, quality of life.
References
mPFS
First-line KISQALI® +AI showed a significant PFS benefit over combination CT in patients with clinically aggressive HR+/HER2- mBC*1
References
Tumor response
KISQALI® matches the tumour response rates seen with combination CT1
References
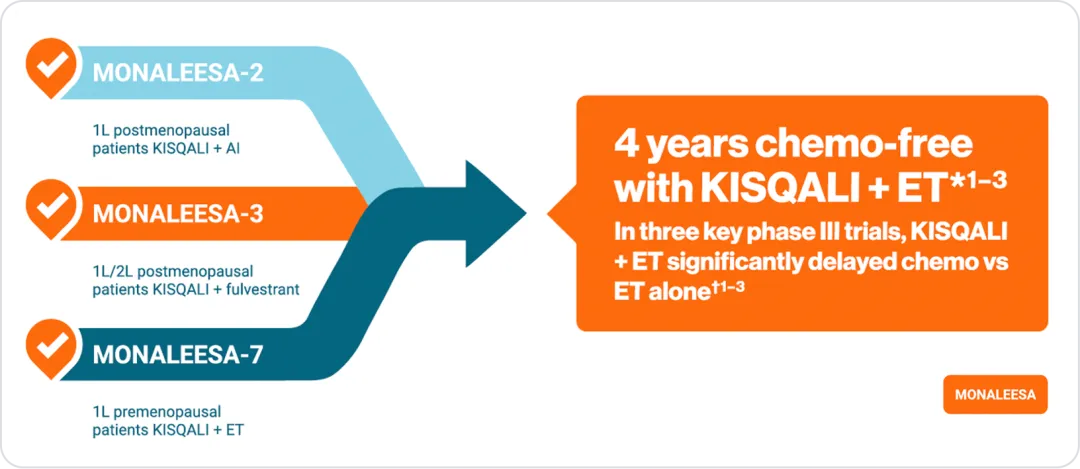
Chemo delay
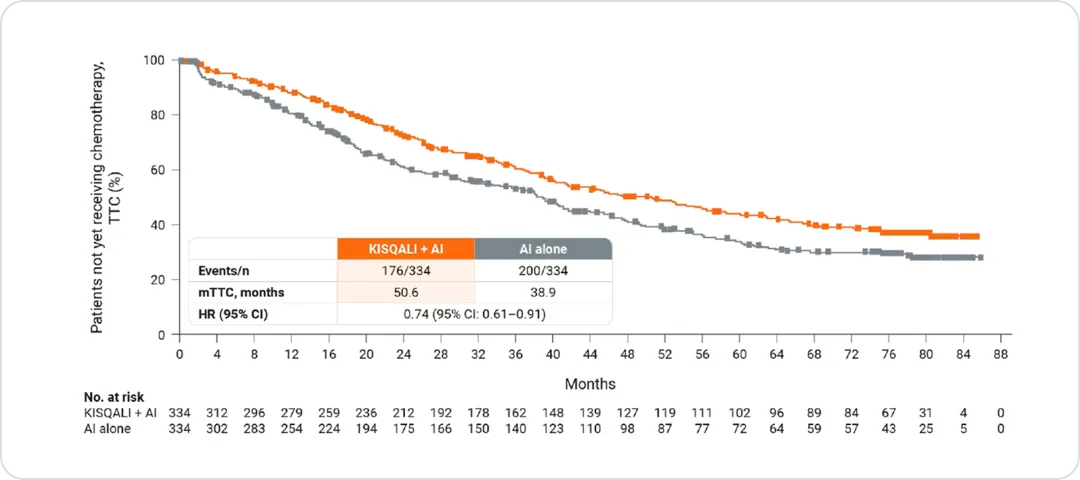
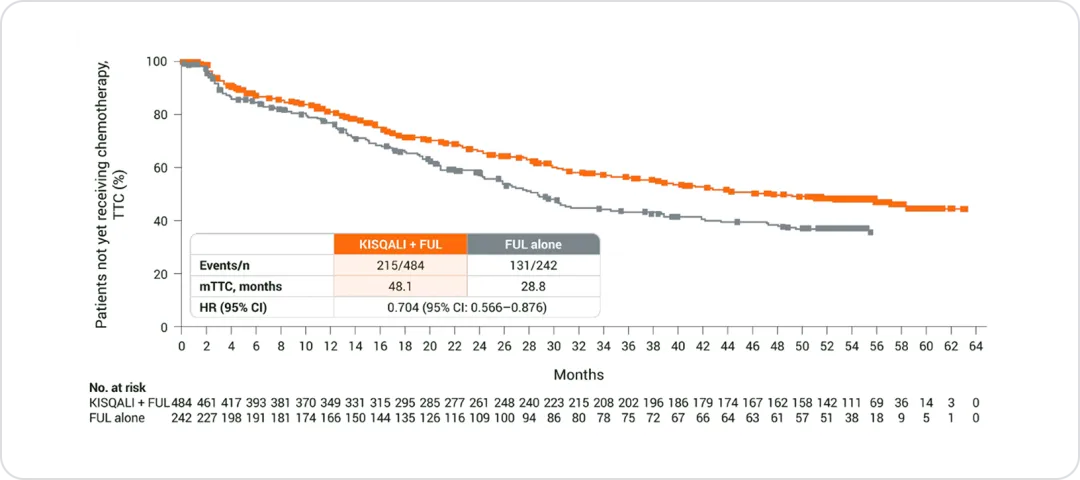
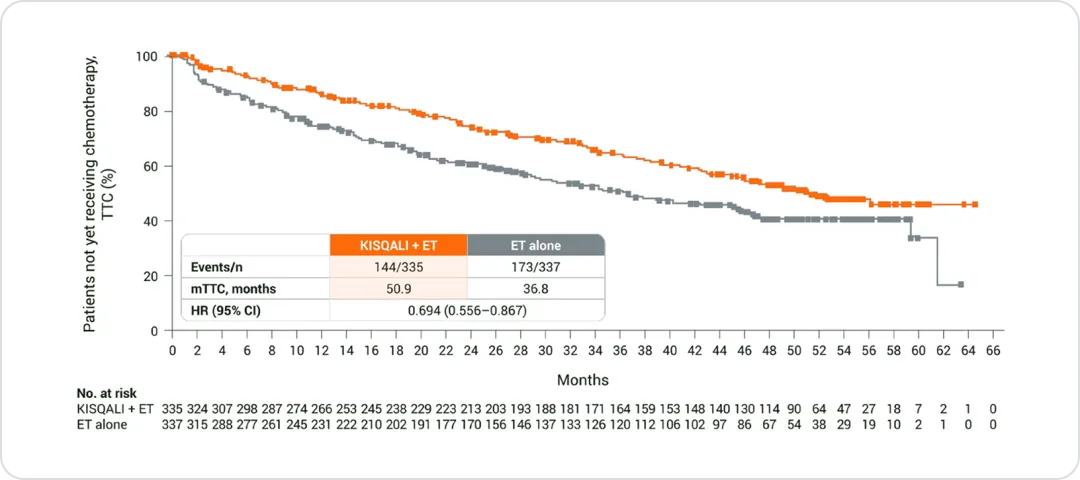
With KISQALI®, you can help your patients delay chemo1–3
KISQALI® + ET consistently delayed the need for chemo across all three phase III trials1–3
The significant benefit of KISQALI® is extended to patients with liver metastases in a pooled ML analysis4
📍 Patients with liver mets derived significant OS benefit with KISQALI® + ET vs. ET
📍 In 1L patients, mOS numerically favored KISQALI® + ET
📍 Approximately 21% of 1L patients had liver metastases
MONALEESA-2: N=668, double-blind, placebo-controlled, 1:1 randomised, multicentre, phase III trial in postmenopausal women with HR+/HER2− aBC. As 1L in advanced disease. No prior ET for aBC and no previous systemic chemotherapy for advanced disease. KISQALI® 600 mg or placebo orally once daily (3 weeks on/1 week off) + AI (letrozole 2.5 mg continuous). The primary endpoint was locally assessed PFS, and the key secondary endpoint was OS. Other secondary endpoints included the ORR (complete or partial response), the CBR (overall response plus stable disease lasting 24 weeks or more), safety, and QoL assessments.1,5
MONALEESA-3: N=726, double-blind, placebo-controlled, 2:1 randomised, phase III trial. As 1L and 2L in advanced disease plus those with early relapse in postmenopausal women with HR+/HER2– aBC. KISQALI® 600 mg or placebo orally once daily (3 weeks on/1 week off) + 500 mg intramuscular fulvestrant. The primary endpoint was locally assessed PFS. Secondary endpoints included OS, ORR, CBR, safety, and tolerability. 1L defined as: Newly diagnosed
(de novo) aBC patients or patients with relapse >12 months from completion of neoadjuvant ET with no treatment for aBC or metastatic disease. 2L was defined as: Relapse on or within 12 months from completion of neoadjuvant ET with no treatment for advanced or metastatic disease (early relapse); relapse >12 months from completion of neoadjuvant therapy with subsequent progression after one line of ET for advanced or metastatic disease, and advanced or metastatic breast cancer at diagnosis that progressed after one line of ET for advanced disease with no prior neoadjuvant treatment for early disease.2,6
MONALEESA-7: N=672, double-blind, placebo-controlled, 1:1 randomised, phase III trial in pre- or perimenopausal women with HR+/HER2− aBC. As 1L in advanced disease and in patients who received 1 or fewer lines of chemotherapy for aBC. KISQALI® 600 mg or placebo orally once daily (3 weeks on/1 week off) + AI (letrozole 2.5 mg or anastrozole 1 mg) or tamoxifen* 20 mg orally once daily continuously + LHRH agonist (goserelin 3.6 mg subcutaneously on day 1 of every cycle). The primary endpoint was investigator-assessed PFS. The key secondary endpoint was OS, defined as the time from randomisation to death from any cause.3
•KISQALI® should not be co-administered with tamoxifen.7
1L, first-line; 2L, second-line; aBC, advanced breast cancer; AI, aromatase inhibitor; CBR, clinical benefit rate; chemo, chemotherapy; CI, confidence interval; ET, endocrine therapy; HER2-, human epidermal growth factor receptor 2 negative; HR, hazard ratio; HR+, hormone receptor positive; LHRH, luteinising hormone-releasing hormone; ORR, overall response rate; OS, overall survival; PFS, progression-free survival; QoL, quality of life; TTC, time to chemotherapy.
References
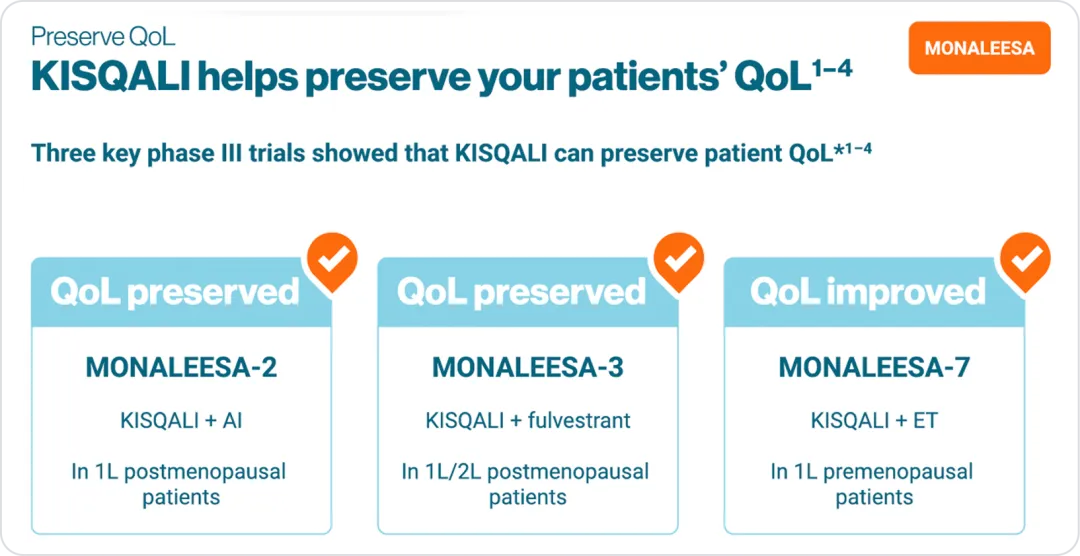
QoL
MONALEESA
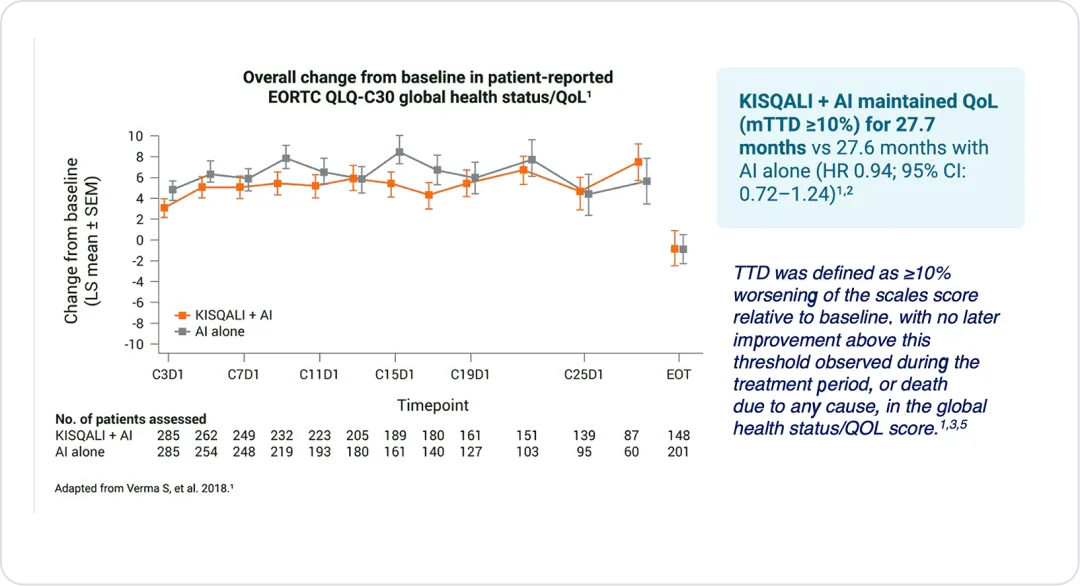
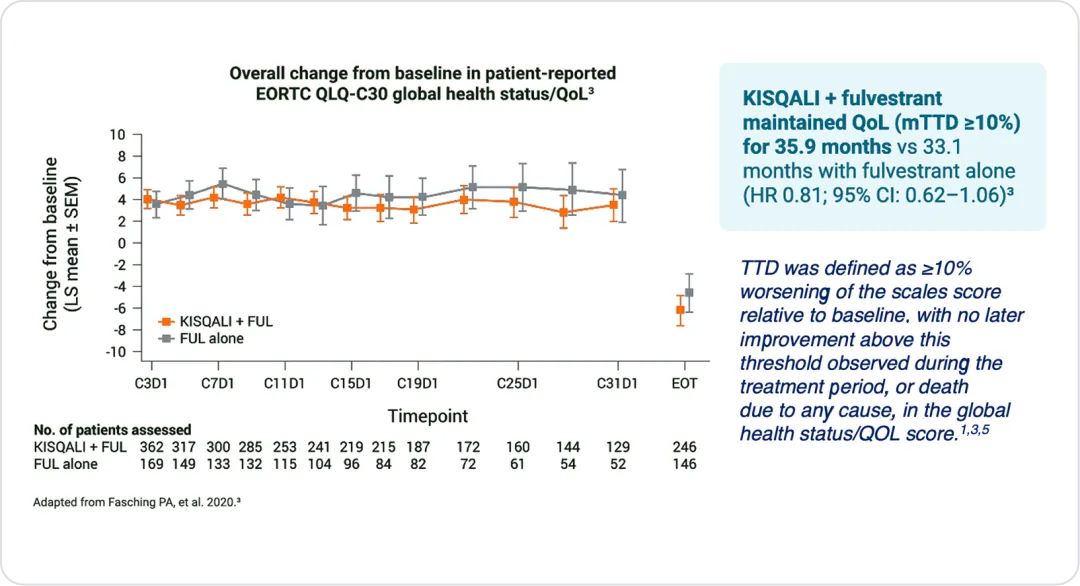
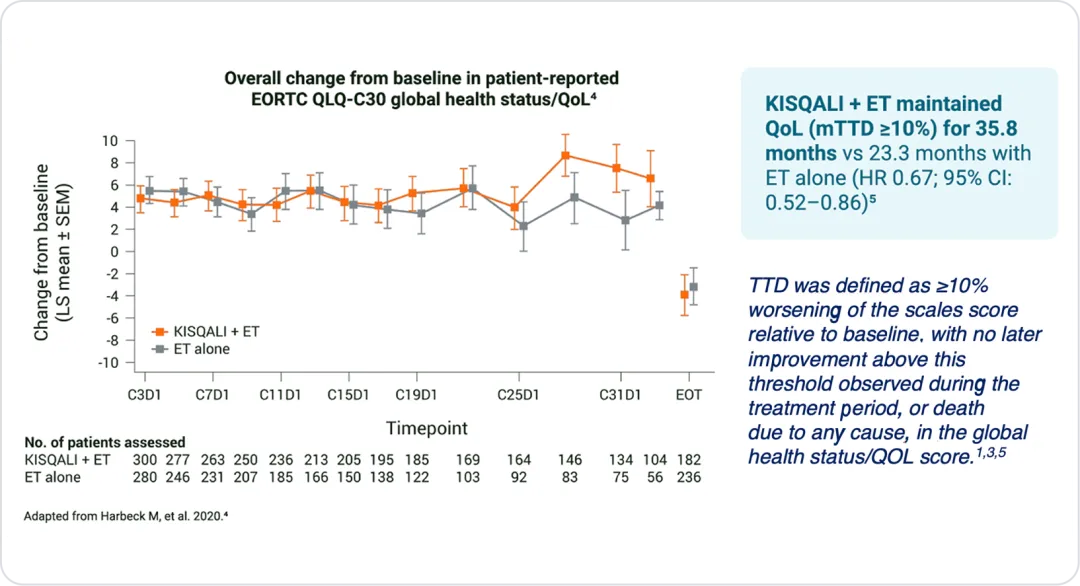
KISQALI® + ET consistently preserved QoL across all three phase III trials1–5
MONALEESA-2: N=668, double-blind, placebo-controlled, 1:1 randomised, multicentre, phase III trial in postmenopausal women with HR+/HER2− aBC. As 1L in advanced disease. No prior ET for aBC and no previous systemic chemotherapy for advanced disease. KISQALI® 600 mg or placebo orally once daily (3 weeks on/1 week off) + AI (letrozole 2.5 mg continuous). The primary endpoint was locally assessed PFS, and the key secondary endpoint was OS. Other secondary endpoints included the ORR (complete or partial response), the CBR (overall response plus stable disease lasting 24 weeks or more), safety, and QoL assessments.5
MONALEESA-3: N=726, double-blind, placebo-controlled, 2:1 randomised, phase III trial. As 1L and 2L in advanced disease plus those with early relapse in postmenopausal women with HR+/HER2– aBC. KISQALI® 600 mg or placebo orally once daily (3 weeks on/1 week off) + 500 mg intramuscular fulvestrant. The primary endpoint was locally assessed PFS. Secondary endpoints included OS, ORR, CBR, safety, and tolerability. 1L defined as: Newly diagnosed (de novo) aBC patients or patients with relapse >12 months from completion of neoadjuvant ET with no treatment for aBC or metastatic disease. 2L was defined as: Relapse on or within 12 months from completion of neoadjuvant ET with no treatment for advanced or metastatic disease (early relapse); relapse >12 months from completion of neoadjuvant therapy with subsequent progression after one line of ET for advanced or metastatic disease, and advanced or metastatic breast cancer at diagnosis that progressed after one line of ET for advanced disease with no prior neoadjuvant treatment for early disease.6
MONALEESA-7: N=672, double-blind, placebo-controlled, 1:1 randomised, phase III trial in pre- or perimenopausal women with HR+/HER2− aBC. As 1L in advanced disease and in patients who received 1 or fewer lines of chemotherapy for aBC. KISQALI® 600 mg or placebo orally once daily (3 weeks on/1 week off) + AI (letrozole 2.5 mg or anastrozole 1 mg) ortamoxifen* 20 mg orally once daily continuously + LHRH agonist (goserelin 3.6 mg subcutaneously on day 1 of everycycle). The primary endpoint was investigator-assessed PFS. The key secondary endpoint was OS, defined as the time from randomisation to death from any cause.7
•KISQALI® should not be co-administered with tamoxifen.8
1L, first-line; 2L, second-line; AI, aromatase inhibitor; aBC, advanced breast cancer; CBR, clinical benefit rate; CI, confidence interval; EORTC QLQ-C30, European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire; ET, endocrine therapy; HER2-, human epidermal growth factor receptor 2 negative; HR, hazard ratio; HR+, hormone receptor positive; LHRH, luteinising hormone-releasing hormone; mTTD, median time to deterioration; ORR, overall response rate; OS, overall survival; PFS, progression-free survival; QoL, quality of life; TTD, time to deterioration
References
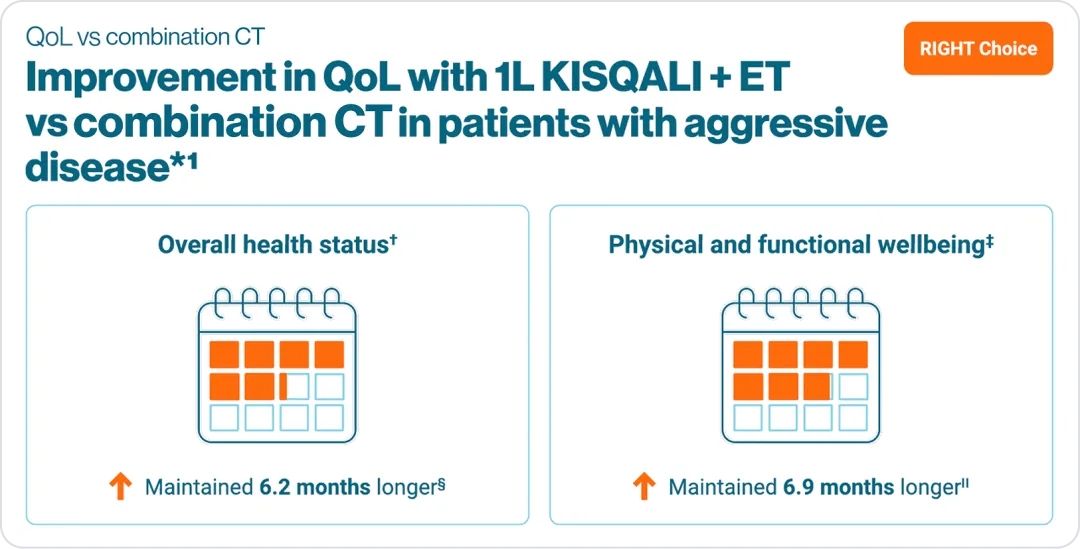
RIGHT CHOICE
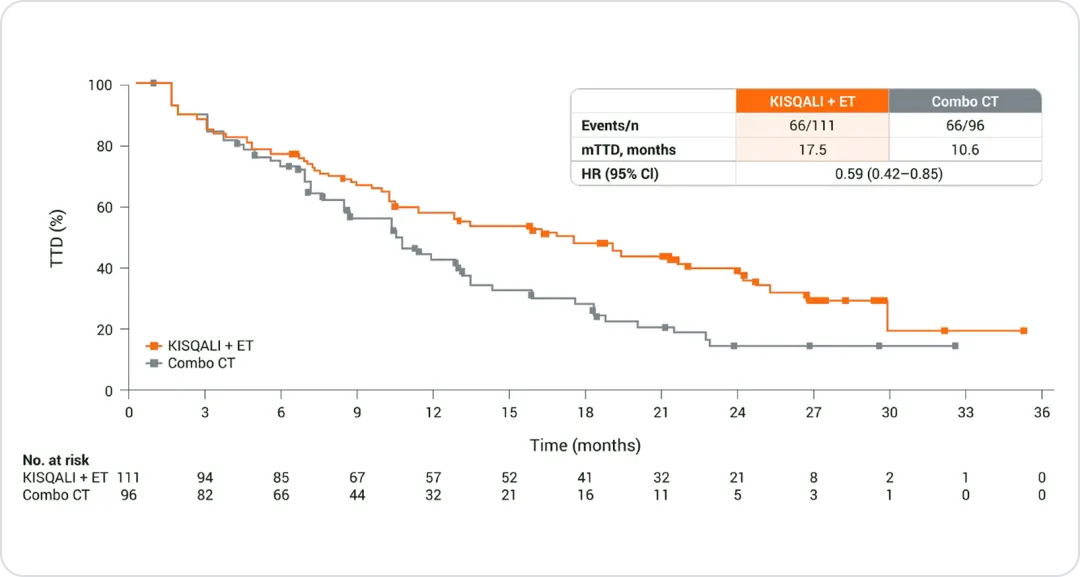
1L KISQALI® + ET is associated with improvements in QoL vs. combination CT in patients with aggressive disease*1
*Aggressive disease features included symptomatic visceral metastases, rapid disease progression or impending visceral compromise, or markedly symptomatic non-visceral disease.2
†mTTD based on the composite endpoint for overall health status score.1
‡mTTD based on a ≥10% decrease in composite endpoint for TOI score.1
§HR 0.63; 95% CI: 0.44–0.90.1
IIHR 0.59; 95% CI: 0.42–0.85.1
1L, first-line; CI, confidence interval; combo CT, combination chemotherapy; ET, endocrine therapy; HR, hazard ratio; mTTD, median time to deterioration;
QoL, quality of life; mTTD based TOI, trial outcome index.
References
KISQALI® NSS - UAE
KISQALI® NSS - UAE