Image

Image
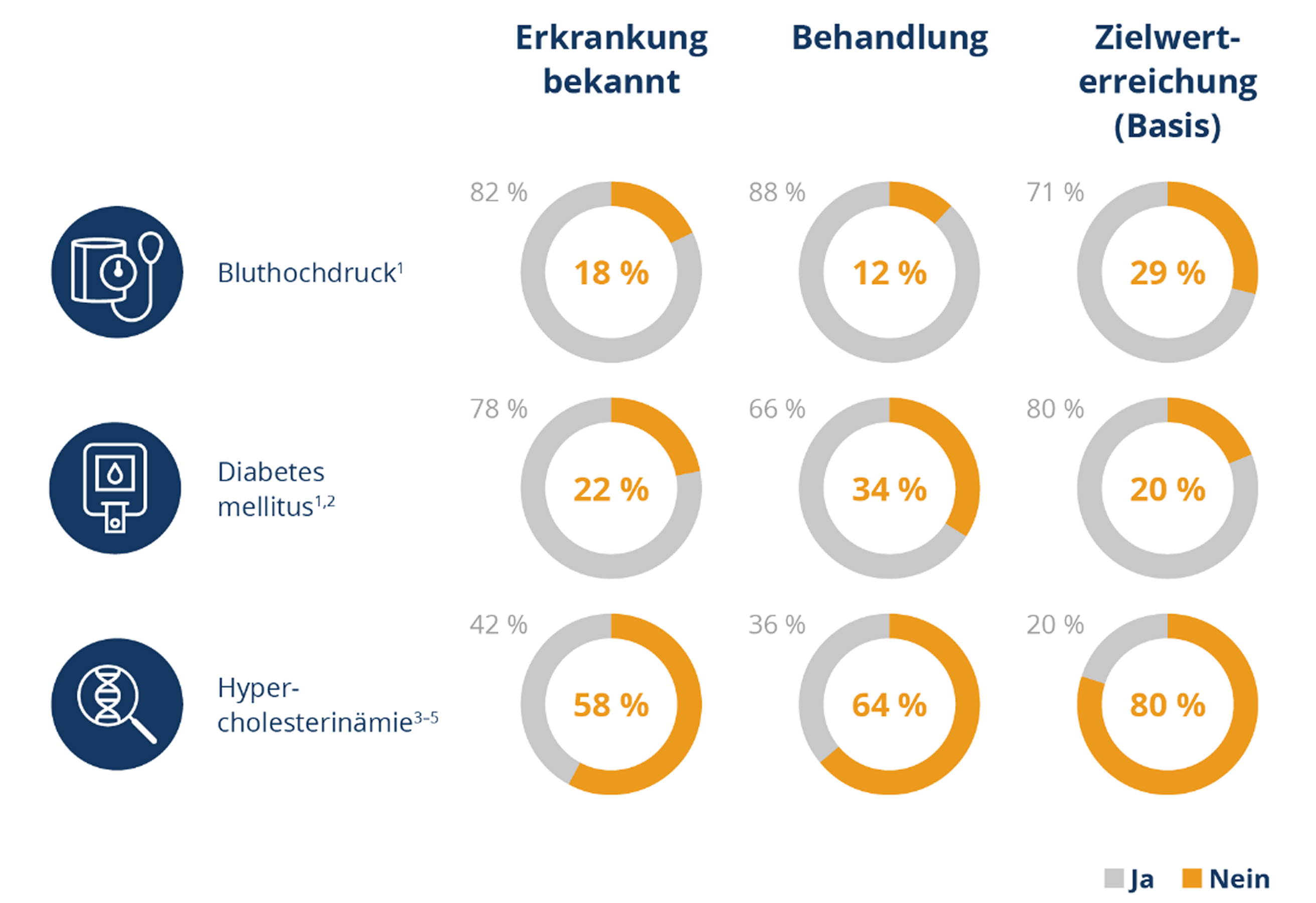
Diagnose-, Behandlungs- und Zielwerterreichung bedeutender Risikofaktoren für kardiovaskuläre Ereignisse. Abbildung modifiziert nach Referenzen 1–5.
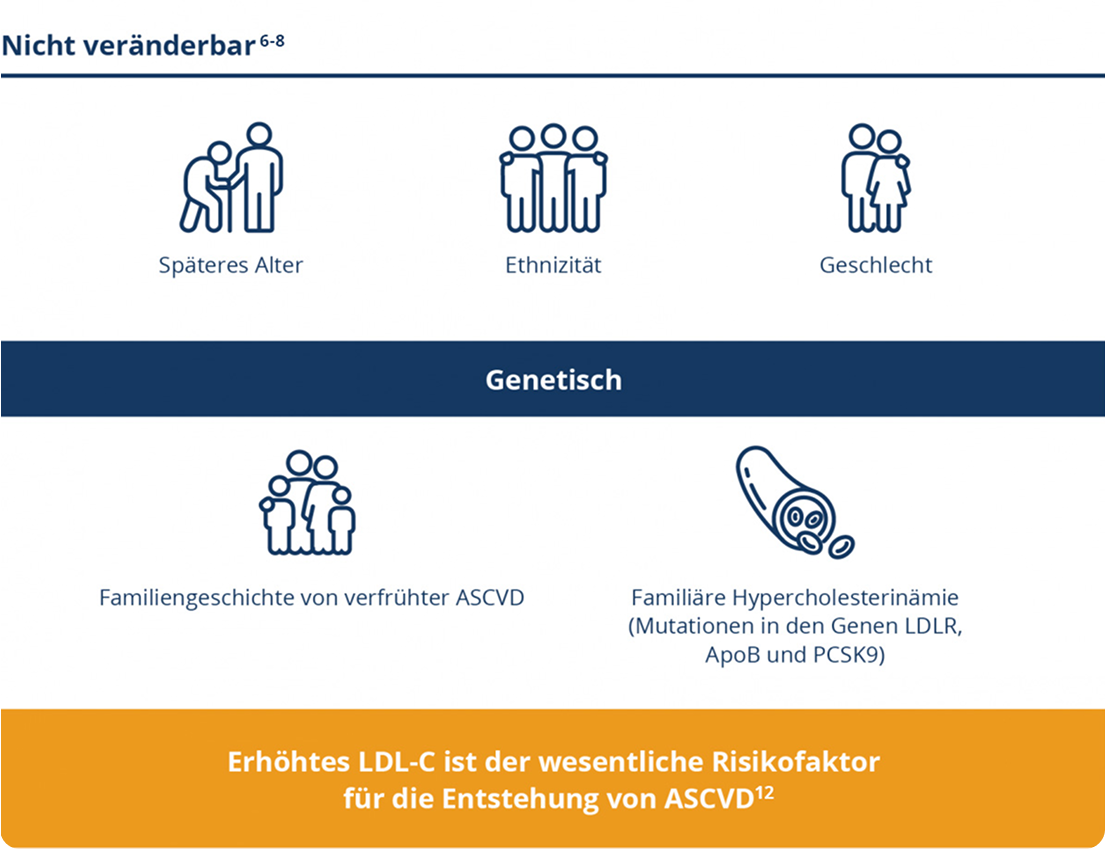
Risikofaktoren
Die meisten Fälle von ASCVD sind auf potenziell veränderbare Risikofaktoren zurückzuführen.
Referenzen
- Neuhauser, H.K., et al., Hypertension prevalence, awareness, treatment and control in Germany 1998 and 2008–2011. J Hum Hypertens. 2015;29(4): p. 247–53. https://doi.org/10.1038/jhh.2014.82.
- Du, Y., et al., Changes in diabetes care indicators: findings from German National Health Interview and Examination Surveys 1997–1999 and 2008–2011. BMJ Open Diabetes Res Care. 2015;3(1):e000135. https://doi.org/10.1136/bmjdrc-2015-000135.
- Scheidt-Nave, C., et al., Bundesgesundheitsblatt – Gesundheitsforschung – Gesundheitsschutz. 2013;56(5-6): p. 661–7. German. https://doi.org/10.1007/s00103-013-1670-0.
- März, W., et al., Utilization of lipid-modifying therapy and low-density lipoprotein cholesterol goal attainment in patients at high and very-high cardiovascular risk: Real-world evidence from Germany. Atherosclerosis. 2018;268: p. 99–107. https://doi.org/10.1016/j.atherosclerosis.2017.
- Fox, K.M., et al., Treatment patterns and low-density lipoprotein cholesterol (LDL-C) goal attainment among patients receiving high- or moderate-intensity statins. Clin Res Cardiol. 2018;107(5): p. 380–88. https://doi.org/10.1007/s00392-017-1193-z.
- Mach, F., et al., 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J, 2020. 41(1): p. 111–88.
- Grundy, S.M., et al., 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology / American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology, 2019. 73(24): p. e285–e350.
- Jernberg, T., et al., Cardiovascular risk in post-myocardial infarction patients: nationwide rea- world data demonstrate the importance of a long-term perspective. European Heart Journal, 2015. 36(19): p. 1163–170.
- Langlois, M.R., et al., Quantifying atherogenic lipoproteins: current and future challenges in the era of personalized medicine and very low concentrations of LDL cholesterol. A consensus statement from EAS and EFLM. Clinical Chemistry, 2018. 64(7): p. 1006–33.
- Holmes, M.V., and Ala-Korpela, M., What is ‘LDL cholesterol’? Nature Reviews Cardiology, 2019. 16(4): p. 197–8.
- http://www.agla.ch/de/rechner-und-tools/agla-risikorechner (aufgerufen am 7.8.2024)
- Ference, B.A., et al., Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. European Heart Journal, 2017. 38(32): p. 2459–72.
- Ference, B.A., et al., Impact of Lipids on Cardiovascular Health: JACC Health Promotion Series. J Am Coll Cardiol, 2018. 72(10): p. 1141–56.
- Nicholls, M.G., Richards, A.M., and Christchurch, G., Cardioendocrine Research, Disease- monitoring of patients with chronic heart failure. Heart, 2007. 93(4): p. 519–23.
- Cholesterol Treatment Trialists, C., et al., Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet, 2010. 376(9753): p. 1670–81.
- Silverman, M.G., et al., Association Between Lowering LDL-C and Cardiovascular Risk Reduction Among Different Therapeutic Interventions: A Systematic Review and Meta-analysis. JAMA, 2016. 316(12): p. 1289–97.
- Wang, N., et al., Intensive LDL cholesterol-lowering treatment beyond current recommendations for the prevention of major vascular events: a systematic review and meta-analysis of randomised trials including 327 037 participants. Lancet Diabetes Endocrinol, 2020. 8(1): p. 36–49.
- Giugliano, R.P., et al., Clinical efficacy and safety of achieving very low LDL-cholesterol concentrations with the PCSK9 inhibitor evolocumab: a prespecified secondary analysis of the FOURIER trial. Lancet, 2017. 390(10106): p. 1962–1971.
Die aufgeführten Referenzen stellt Novartis auf Anfrage zur Verfügung.